Glenoid fractures, while relatively less common than other orthopedic injuries, pose significant challenges to both patients and healthcare professionals.
The glenoid, being a vital part of the shoulder joint, plays an essential role in the wide range of motion that shoulders are known for.
Detecting and correctly managing these fractures are crucial for a full recovery and return to pre-injury levels of activity.
From recognizing symptoms to exploring recovery pathways, it’s essential to grasp the complexities surrounding these types of shoulder traumas.
Keep reading to learn about the nuances of glenoid fractures and how they’re expertly cared for.
What Are Glenoid Fractures and Why They Matter
When you hear about injuries to your shoulder, glenoid fractures might emerge as a less familiar term.
These fractures, integral to the shoulder’s anatomy, can significantly affect your arm’s mobility and stability.
Imagine the glenoid fossa as a shallow socket in the shoulder blade that cradles the ball of your upper arm bone; a fracture here disrupts this elegant skeletal harmony, curtailing your ability to perform even basic tasks that rely on shoulder movement.
Understanding both the definition and the consequences of glenoid fractures is essential for grasping the scope of shoulder joint injuries and the recovery journey ahead.
Defining Glenoid Fractures in the Context of Shoulder Injuries
Glenoid fractures are a specific type of shoulder fracture that occurs in the glenoid cavity, the part of the scapula (shoulder blade) that forms the socket of the shoulder joint. These fractures disrupt the normal articulation between the scapula and the humerus, the bone of the upper arm, potentially compromising the joint’s function and stability.
Such an injury can occur through various forms of trauma, whether from a sports injury, a fall, or a sudden impact. A fracture in this area can lead to a cascade of shoulder joint injuries, necessitating a thorough assessment and precise treatment to restore functionality and prevent long-term complications involving the humerus.
The Impact of Glenoid Fractures on Shoulder Functionality
The integrity of your shoulder hinges on the pristine condition of the glenoid — any fracture to this area can cause profound disruptions to your daily life. A compromised glenoid impacts the complex interplay of muscles, ligaments, and bones essential for shoulder stability and arm rotation, leading to pain and a hampered range of motion.
Your swift access to comprehensive care becomes critical, as neglecting a glenoid fracture risks early arthritis, recurrent dislocations, and a gradual decline in the functionality of your shoulder. Initiating prompt treatment is paramount to ensuring a return to optimal mobility and minimizing future complications.
Identifying the Symptoms of a Glenoid Fracture
Recognizing the onset of a glenoid fracture can be a cryptic task, as symptoms often resemble other shoulder joint injuries.
You’ll want to pay close attention to pain patterns, which can serve as tell-tale signs of such fractures.
Experiencing acute discomfort upon specific arm movements or when applying pressure around the shoulder suggests that the glenoid may be compromised.
Vigilance is also required to spot other indicators that might point to a glenoid fracture, including swelling, bruising, and an inability to move the shoulder through its full range of motion.
Detecting these signals early can expedite diagnosis and set you on the path to a structured treatment protocol.
Recognizing Pain Patterns Specific to Glenoid Injuries
When dealing with potential glenoid injuries, your body’s signals merit your undivided attention. A piercing pain that strikes as you reach overhead or a staunch ache when you attempt to sleep could pinpoint a fracture within the glenoid’s contours.
Additionally, if your shoulder betrays a subtle crunching or grinding sensation during certain movements or if you notice an abrupt limitation to your range of motion, it’s prudent to consider these as red flags. Such discomfort, indicative of underlying glenoid damage, necessitates immediate medical scrutiny.
Other Key Indicators That You Might Have a Glenoid Fracture
Should your shoulder swell like a balloon and endures severe pain with even the slightest jostle, or bruising manifests, consider these as potential harbingers of a glenoid fracture, urging a swift evaluation by a healthcare provider.
Perhaps you’ve noticed your shoulder doesn’t quite sit right, looking deformed or out of place; such a visible irregularity can be a strong indication of a glenoid break. Deformity, coupled with an acute inability to use the shoulder joint due to pain– such as struggling to raise your arm or carry objects – should prompt you to seek out an orthopedic specialist’s insight without delay.
The Usual Causes Behind Suffering a Glenoid Fracture
Grasping the origins of a glenoid fracture is key in both prevention and treatment.
Such fractures typically result from traumatic events which apply direct force or stress to the shoulder complex, potentially shattering the intricate balance maintained by the glenoid socket.
Beyond accidents and sports-related mishaps, a range of activities and underlying conditions can escalate your risk for this type of injury.
Recognize how your daily actions might contribute to the likelihood of experiencing a glenoid fracture, and understand the preemptive measures that could safeguard the well-being of your shoulder joint.
Traumatic Events Leading to Most Glenoid Fractures
Consider the abrupt forces at play in high-velocity collisions or when falling from a height; these are prevalent situations that can produce a glenoid fracture. Motor vehicle accidents, for instance, often involve rapid deceleration or blunt force trauma to the shoulder area, risking severe disruption to the glenoid cavity’s integrity.
Sporting scenarios make up another common backdrop for this type of shoulder injury. Contact sports such as football, rugby, or hockey can put you in the line of intense impact, risking direct blows to the glenoid, while falls during skiing or skateboarding can impose significant strain on the shoulder, leading to fractures.
Activities and Conditions That Increase Your Risk
Engaging in activities with repetitive overhead motions, like painting or playing volleyball, gradually exhausts your shoulder’s capacity, which can prime it for potential fractures. Your occupation or hobbies might predispose you to stress-related injuries in the glenoid, making awareness and preventive strategies critical to protecting your shoulder health.
Furthermore, medical conditions such as osteoporosis diminish the density and strength of your bones, elevating your vulnerability to glenoid fractures even from minor falls or impacts. Knowing your bone health status and discussing with your healthcare provider can lead to informed lifestyle choices to bolster your skeletal resilience.
Diagnostic Procedures for Confirming a Glenoid Fracture
Once you suspect a glenoid fracture, pinpointing the precise nature of the injury is your next critical step.
Your journey to recovery begins with a thorough diagnosis where healthcare professionals employ a blend of keen clinical acumen and state-of-the-art technology.
Let’s explore the initial assessment techniques that set the stage for a clear understanding of your condition and the advanced imaging tests that bring the specifics of your injury into sharp relief.
Initial Assessment Techniques Used by Healthcare Professionals
When you arrive with a potential glenoid fracture, healthcare professionals commence an evaluation with a detailed clinical history and physical examination. They’ll carefully scrutinize your recounting of the incident, assess your pain levels, and observe the range of motion and stability of your shoulder to gauge the likelihood of a fracture.
Following the initial discussion, your healthcare provider will conduct a hands-on assessment, palpating the shoulder region to locate areas of tenderness, deformity, or swelling that signal the site of a humerus fracture. This tactile approach aids in delineating the extent of your injury before moving forward with imaging tests.
Advanced Imaging Tests to Precisely Identify the Injury
Embarking on the diagnostic quest, your medical team often turns to X-rays as the first foray into visualizing the injury. While X-rays are excellent for detecting breaks in bone continuity, they may not provide a thorough view of complex glenoid fractures, leading practitioners to recommend more sophisticated imaging studies.
Should the X-ray suggest anomalies or if the healthcare professionals seek a more intricate picture, computed tomography (CT) scans come into play. A CT scan offers a multidimensional glimpse of your glenoid, revealing details undetected by X-rays, such as the precise type and extent of the fracture, whether it be displaced or non-displaced, and if there are any associated injuries, setting a definitive course for your treatment regimen.
Treatment Options Available for Recovering From a Glenoid Fracture
Addressing a glenoid fracture promptly and effectively is vital to healing and regaining the full use of your shoulder. Depending on the severity and type of fracture sustained, you may be presented with either nonsurgical or surgical treatment options by your healthcare provider. Nonsurgical methods usually involve immobilization with a sling or brace, giving the bone time to heal naturally, while more severe fractures might necessitate orthopedic surgery intervention to realign and stabilize the bone fragments.
Your treatment begins with a careful evaluation of the injury. If your fracture is non-displaced, meaning the bones remain in alignment, a regimen of rest and restricted movement may allow for natural healing. During this period, managing pain and inflammation is crucial to maintaining comfort and encouraging recovery.
Surgery becomes a consideration when you have a displaced or complicated fracture involving multiple bone pieces or if the injury affects the stability of your shoulder joint. Your surgeon might employ plates, screws, or anchors to secure the bones in their proper place, enabling the restoration of shoulder anatomy and function. After surgery, a period of immobilization is necessary to support the healing process.
Following the initial treatment phase, rehabilitation plays a pivotal role in your recovery. A tailored physical therapy program focuses on gradually restoring strength and range of motion to your shoulder. Persistence and dedication to your rehabilitation exercises will be critical, as they significantly impact your ability to return to normal activities and prevent future shoulder issues.
4 Glenoid Fracture Descriptions
As you navigate the complexities of shoulder joint injuries, knowing the specific type of fracture you’re dealing with can propel your understanding and streamline your path to recovery.
Glenoid fractures are categorized by their location and the pattern of the break within the bone, each type presenting unique challenges and treatment avenues.
Your orthopedic specialist may identify any multitude of these fractures such as Impaction Fractures, where the bone is driven into another, and the more straightforward classifications of Displaced and Non-displaced Fractures, denoting bone alignment post-injury.
Grasping these terms enhances your dialogue with healthcare providers and empowers your active role in the treatment and healing process.
Comminuted Fracture:
A comminuted fracture presents as one of the more serious challenges among the types of glenoid fractures. In your case, this means the glenoid bone is fragmented into three or more pieces, complicating both stabilization and the healing process.
Your treatment may become complex, often involving surgical intervention to reconstruct the fractured bone elements. Restoring the original structure of your shoulder joint becomes a priority to prevent long-term mobility issues and maintain shoulder function.
Impaction Fracture:
Should you face an impaction fracture, it implies a bone has been driven into another, often due to compression or a fall onto an outstretched hand. This type of glenoid fracture sometimes doesn’t present with visually obvious deformity but can cause significant pain and functional impairment in your shoulder.
Your orthopedic care provider will scrutinize this injury meticulously, gauging its impact on your shoulder’s anatomy. It’s not uncommon for treatment to involve a period of immobilization, allowing the impacted bone to settle back into position and fostering recovery with minimal invasiveness.
Displaced Fracture:
Encountering a displaced fracture implies that the bone fragments have been forced out of their original alignment, posing a notable hurdle in your journey to rehabilitation. This condition often arises from high-energy impacts or falls that not only fracture the glenoid but also disrupt the intricate articulation of the shoulder joint.
Addressing a displaced fracture swiftly is essential, as improper alignment can lead to impaired shoulder mechanics and chronic joint issues. Your orthopedic surgeon’s skilled hands will likely intervene, using advanced techniques to realign the bone pieces and stabilize them, ensuring the foundation for your shoulder’s successful recovery is set in place.
Non-displaced Fracture:
A non-displaced fracture means that, despite a break in the glenoid bone, the pieces remain in correct alignment, offering a less complex road to healing. You can breathe a little easier knowing that this type often heals with conservative treatment, bypassing the need for surgical intervention to reposition bone fragments nerve.
Your focus with a non-displaced fracture revolves around allowing your body the necessary time to undertake its natural healing process. Rest and a strategic period of immobilization will likely form the cornerstone of your recovery, paired with careful monitoring by your healthcare provider to ensure the fracture heals appropriately.
Conclusion
Glenoid fractures disrupt the shoulder’s intricate balance, necessitating immediate attention and precise care to restore functionality. Recognizing the signs and symptoms of these fractures enables timely diagnosis and averts potential long-term joint complications.
A variety of treatment methods, including conservative care or surgery, are tailored to the specific nature of the fracture, underscoring the need for specialized medical evaluation.
Ultimately, understanding glenoid fractures empowers individuals to engage actively in their recovery process and to safeguard their shoulder health effectively.
(Photo Credit – Shutterstock/Envato/Adobe)














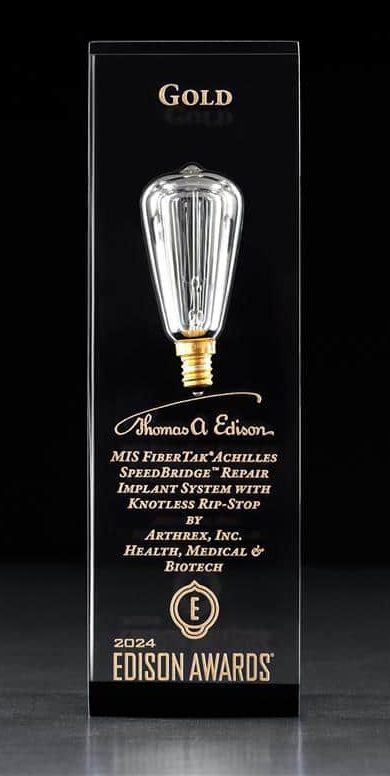 JACKSONVILLE, FL (June 19, 2024) – Not too many doctors can say they have invented something to help their patients. However,
JACKSONVILLE, FL (June 19, 2024) – Not too many doctors can say they have invented something to help their patients. However,